BRCA and Prophylactic Mastectomy (Risk-Reducing Mastectomy)
Most women with breast cancer have what is considered to be a “sporadic” type, which is unrelated to inherited cancer. Approximately 10 to 20 percent of women with a diagnosis of breast cancer have a first degree relative with breast cancer.
For those with a family history of breast cancer, up to 20 percent have a mutation in the breast cancer susceptibility gene, known as BRCA 1 or BRCA 2. Candidates for testing are women with breast cancer diagnosed before age 50, triple-negative breast cancer, two or more primary breast cancers, ovarian cancer, or have Ashkenazi Jewish ancestry. Women with first or second degree relatives who have had breast cancer diagnosed before age 50, in two or more relatives, or ovarian, pancreatic, or prostate cancers are also candidates for testing.
For Breast Reconstruction NYC patients' final determination of candidacy or need for testing should be made by a breast surgeon and/or a breast oncologist, and genetic counseling is recommended. For women that carry the BRCA gene mutation, without a diagnosis of breast cancer, current recommendations are clinical examinations beginning at age 25, annual breast MR scans (MRI) from age 25 – 29, annual mammogram and breast MRI after age 30, risk reducing oophorectomy after child bearing (and/or by age 40), and consideration of risk reducing mastectomy.
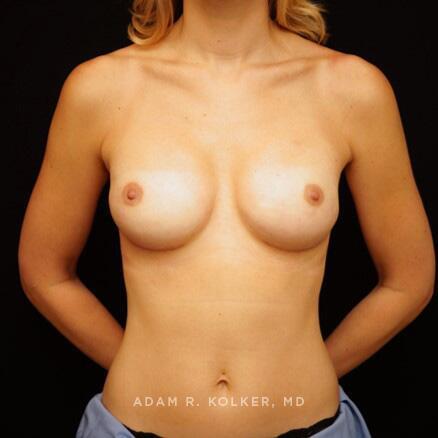
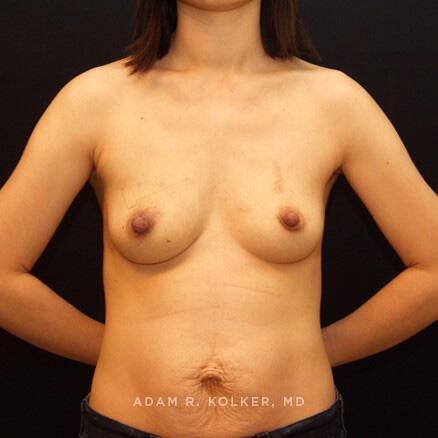
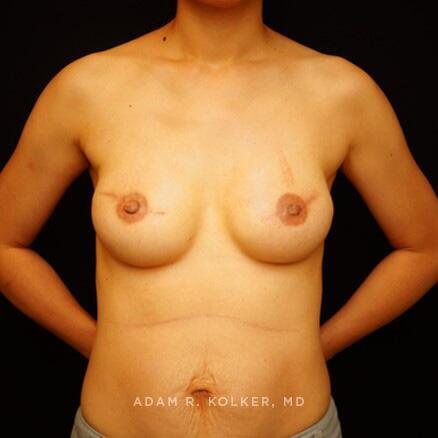
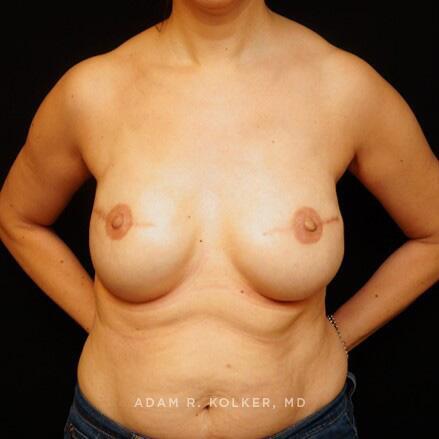
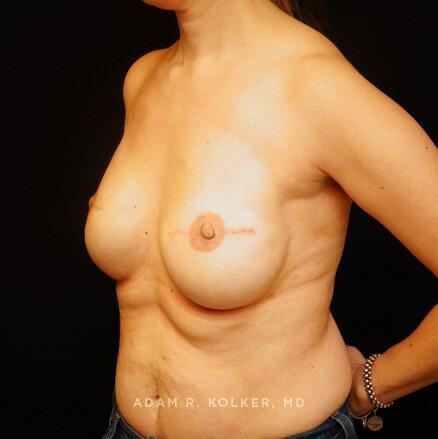
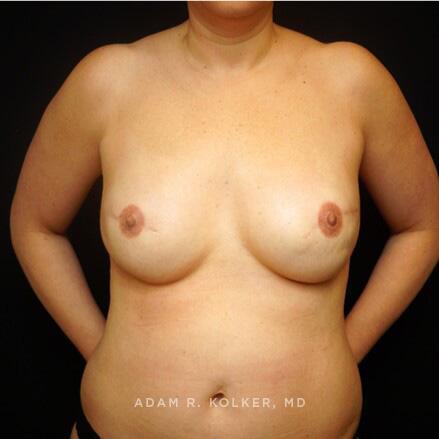
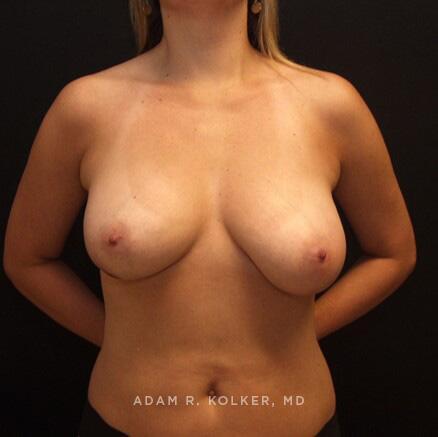
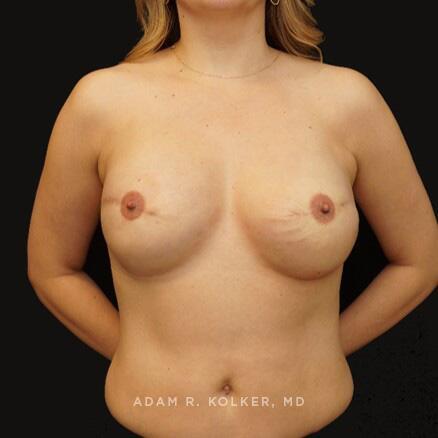
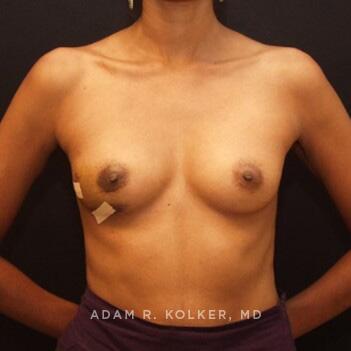
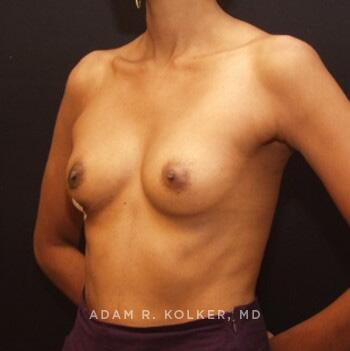
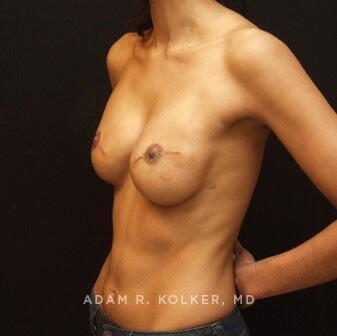
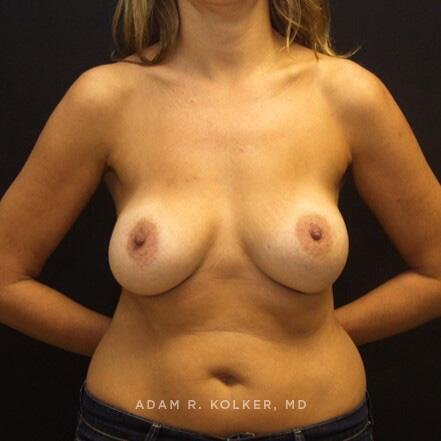
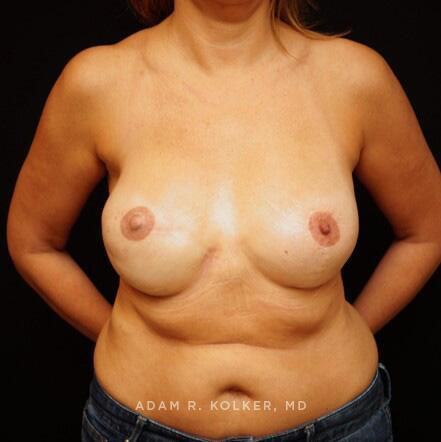
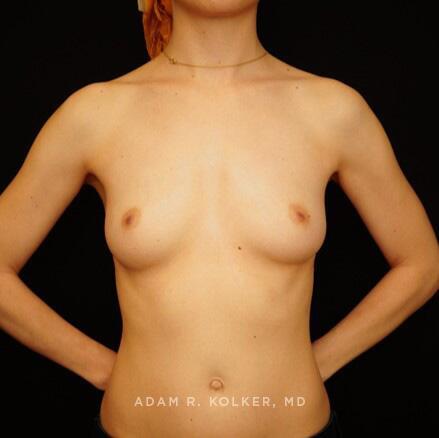
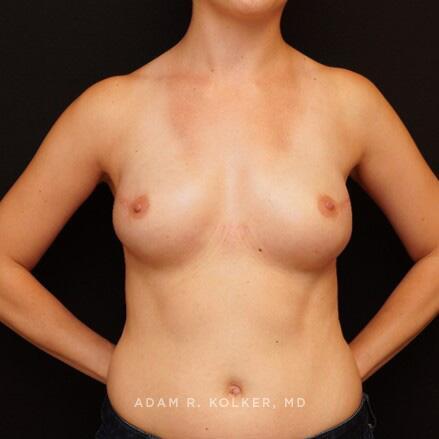
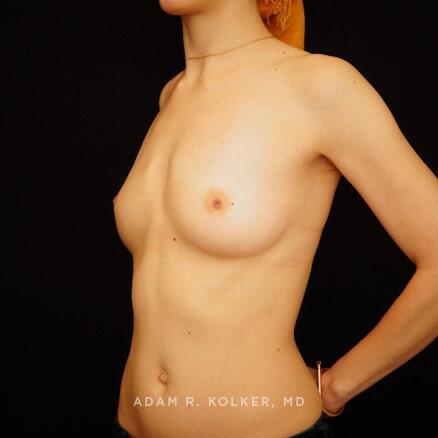
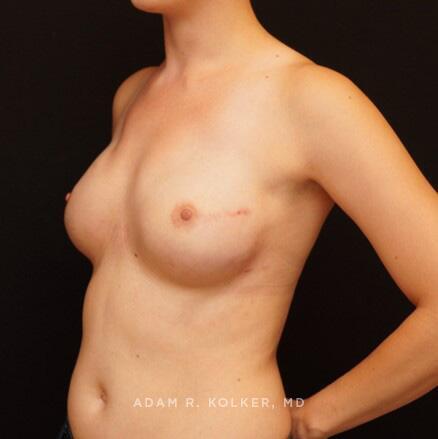
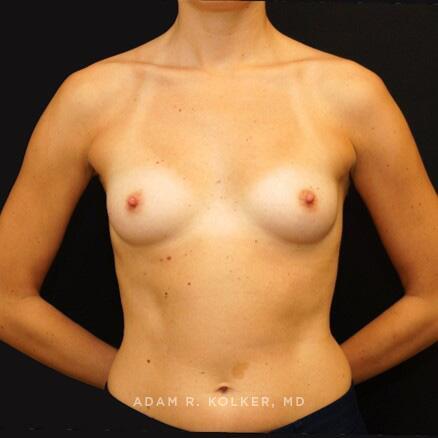
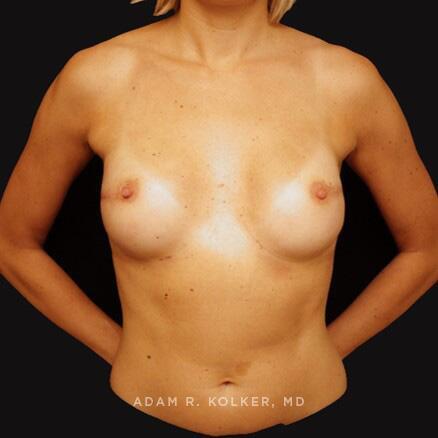
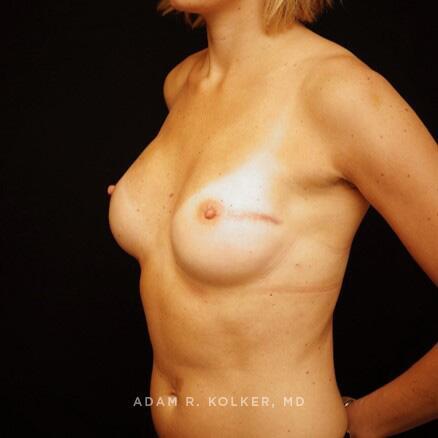
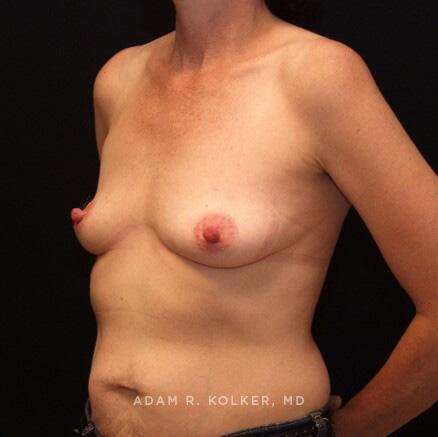
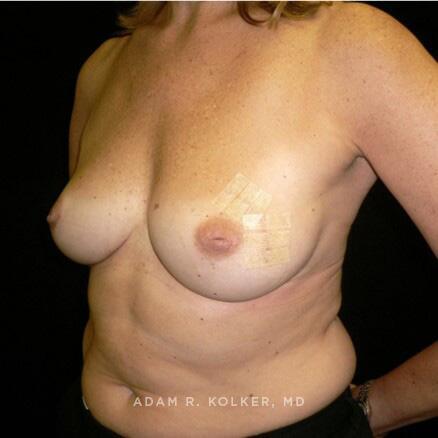
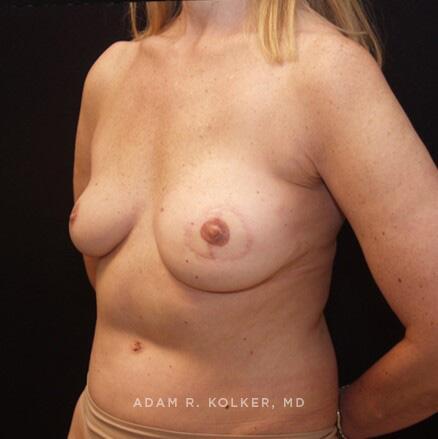
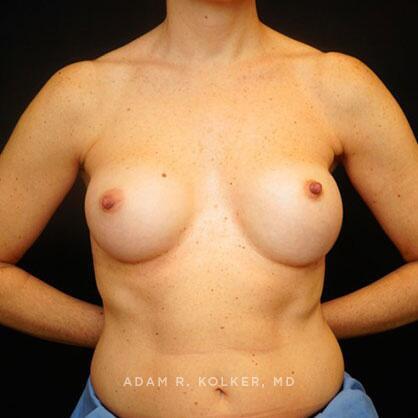
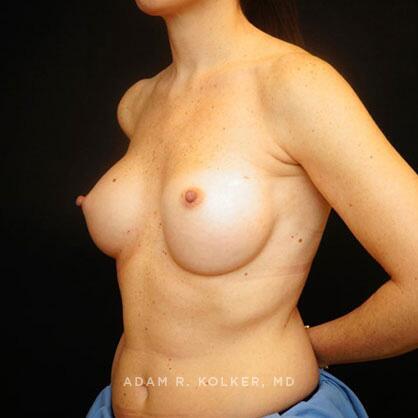
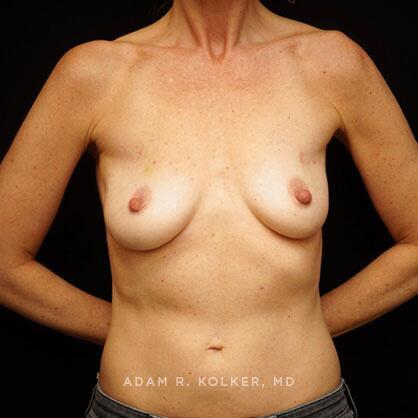
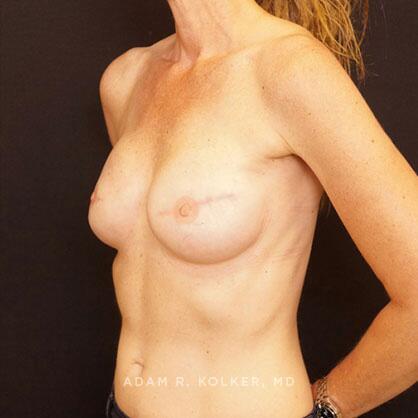
Also known as a prophylactic mastectomy, the decision to undergo surgery must be carefully considered, and is based on personal preference and in depth discussion with your breast surgical oncologist. In retrospective and prospective studies, risk-reducing or prophylactic mastectomy decreases the incidence of breast cancer by 90 percent or more in women who carry the BRCA gene mutation. A bilateral total mastectomy that is skin-sparing, and often nipple sparing, with immediate Breast Reconstruction can be considered.
Oncoplastic Surgery
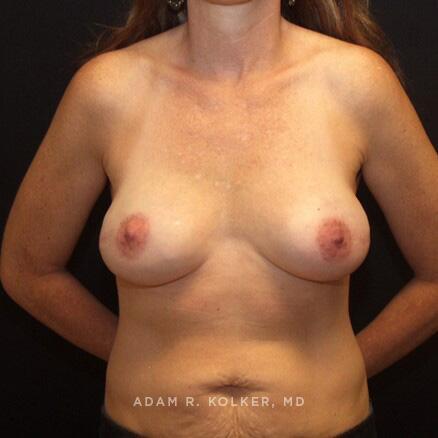
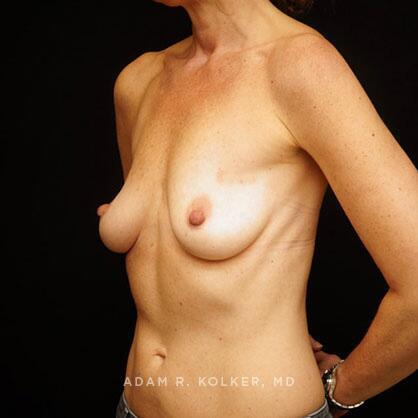
Oncoplastic surgery is a process that falls within the category of breast conservation therapy (BCT), in that the cornerstone of the oncologic surgery is a lumpectomy. Women who are candidates for this procedure generally have a breast size that is fuller (D cup or greater) who desire a breast reduction. During an oncoplastic “reduction”, the most common form of oncoplastic surgery, the lumpectomy region is removed as would be the portion of excess breast tissue that is removed with a breast reduction. The remaining breast tissue can be mobilized and transposed into the region of resection, and the breast is reshaped and lifted. For most women who undergo oncoplastic breast surgery, postoperative radiation is required. While appealing for many women, particularly those with larger breasts, one’s candidacy for oncoplastic surgery is determined by both a breast surgeon and plastic surgeon.
Recovery
Dr. Kolker recommends returning to work 4 weeks following the first stage, although with less physically demanding occupations, some are able to return as early as 3 weeks postop. Drain tubes are usually maintained for 10 – 14 days. Light exercise (cardio without impact) may be resumed after the drains are removed, at approximately the two week point, and more vigorous physical activity may commence four weeks after breast reconstruction surgery. Strength training that excludes pectoralis muscle contraction (including lower body, core, and biceps/triceps toning with arms held below 45 degrees) may resume after 14 - 21 days. The recovery time after the lesser ambulatory stages of the breast reconstruction process is generally 7 to 10 days.
Aftercare
After your Manhattan Breast Reconstruction, follow up visits involve drain and incision line care, drain removal, and tissue expander fills. The fills take a matter of minutes, and while usually performed at two week intervals, they can be spaced at intervals up to 30 days. Dr. Kolker and his nursing staff are available to you at any time during recovery.
Breast Reconstruction in NYC
When considering mastectomy and breast reconstruction, it is critical that you choose a dedicated breast care center, with a surgical team that performs these procedures together on a very frequent basis. Dr. Kolker is an active member of the plastic and reconstructive surgery section at the Dubin Breast Center at Mount Sinai, and works very closely and regularly with the breast surgeons, oncologists, and radiation oncologists. The Dubin Breast Center, providing every facet of comprehensive breast diagnosis and treatment, is committed to exceptional care of women with breast cancer.
The information on this website is meant to provide a broad overview and some of the nuances of breast reconstruction, and of Dr. Kolker’s preferred approaches to the spectrum of procedures after breast conservation therapy and mastectomy. In consideration of each individual’s specific diagnosis, unique anatomy, and personal desires, in-depth evaluation and discussion with an experienced surgical “team”, consisting of a breast surgeon and plastic surgeon at a comprehensive breast center is imperative. To learn more about post-mastectomy Breast Reconstruction in Manhattan, breast reconstruction alternatives, and an extraordinary team approach to superlative breast cancer care and exceptional aesthetic results, we recommend a consultation with Dr. Kolker where he can more thoroughly discuss your options for breast reconstruction with you.